COVID-19 & BRAIN FUNCTIONING
Our social and scientific communities alike have been drastically uprooted since the novel coronavirus impacted the world last December. This article tackles questions regarding COIVD’s effects on the brain, cognition (thinking clarity), and general life functioning related to contracting the coronavirus, as well as discussing the road to recovery (read time: 10 mins)
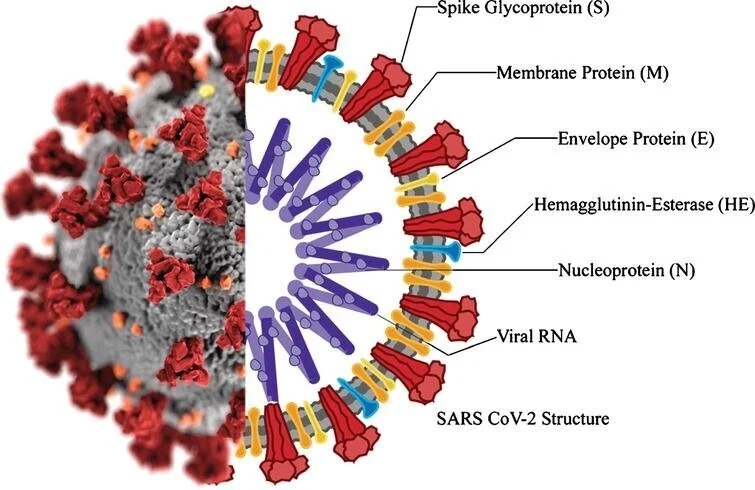
Image credit: Yamamoto, Ariumi, Nishida, Yamamoto, Bauer, Gojobori, Shimotohno, & Mizokami, 2020 (linked)
Side-effects? Am I a long-hauler? What does this illness really look like?
Although the respiratory side effects are readily discussed, research on other significant side effects are now begining to emerge. In fact, a subset of individuals populalry termed “long-haulers” have reported symptoms that continue to affect their lives, even months after they are considered to have “recovered” or produced a negative COVID test. You might have seen the CBS 60 Minutes news special highlighting such cases. Clealry, the range of symptoms is not fully understood, however, here is what we do know:
In one of the largest studies yet, published in The Lancet journal on April 6, 2021, researchers reviewed the records of more than 236,000 COVID-19 patients and found:
34% of COVID-19 patients went on to receive a diagnosis for a neurological or psychological disorder within 6 months of contracting COVID-19.
Apart from COVID alone, the researchers found:
there was a 44% increased risk for neurological and psychological illnesses in COVID patients compared to patients recovering from the flu.
Although mental health symptoms following COVID-19 are generally more common than neurological complications, the seriousness of both symptoms should be considered as society continues to understand this illness, its trajectory, and recovery.
INITIAL NEUROLOGICAL SYMPTOMS
So what are the neurological complications that can occur if one gets sick with COVID-19? The most common neurological symptoms reported include:
Headaches and dizziness
Myalgias (muscle aches and pains)
Encephalopathy (damage or disease that affects the brain)
Dysgeusia (distortion of the sense of taste)
Anosmia (loss of smell)
Impaired cognition (brain fog)
In a study from a large medical center in Chicago, researchers found:
More than 40% of patients with COVID-19 reported having at least one of these symptoms at the outset of treatment, and more than 80% reported having at least one of these symptoms during the course of the illness.
Another initial neurological complication that can sometimes occur is delirium.
Delirium is a syndrome caused by a medical condition (such as COVID-19) and results in acute changes in cognition, attention, and awareness.
In older patients with COVID-19 who present to the emergency room, there is a significant rate of delirium documented (and some of these patients with no other COVID-19 symptoms).
LONG-TERM NEUROLOGICAL CONSEQUENCES
Research continues to suggest that potential long-term consequences may exist for patients, post-COVID. In particular, cases of mild brain damage due to lack of oxygen (hypoxemia), stroke, and encephalitis (brain infection and swelling) have emerged in the literature.
Those over the age of 70 may be most vulnerable to these secondary health risks, as their bodies fight to recover from COVID-19.
Due to these brain insults (e.g., encephalitis, stroke, hypoxemia), profound cognitive impairments can occur. Here are some key points to keep in mind.
most of the time, any COVID-related brain damage is mild
many survivors, however, report extreme fatigue and overall declines in their mental sharpness and ability
These cases may warrant specific investigation from a neuropsychologist
While brain damage can be seen in more severe cases of COVID-19, even mild cases can produce subtle or lingering effects on cognition, as this infection is not fully understood.
The most common finding is that it can lead to difficulties with sustained attention.
Many post-COVID individuals describe a kind of “brain fog” associated with their recovery.
Clinically speaking, brain fog might describe a state of mental confusion or altered mental status — a state of mental functioning that differs significantly from one’s normal range of cognitive ability (or pre-illness baseline).
It is likely that chronic, long-term neuroinflammation can explain these persistent and residual COVID-19 complaints. Such subtle cognitive changes associated with COVID-19 have caused many individuals problems when returning to work and their normal lives. They report that they “just don’t feel completely like themselves.” This can be particularly upsetting for people, as their difficulties may seem largely invisible to others. Furthermore, not all COVID cases behave the same, so it is important to remember:
It may be easy to feel frustrated, discredited, or shrugged-off by acquaintances who may have recovered without a hitch.
Even doctors can may come off as invalidating at times. New information is proliferating at an unprecedented rate, and thus, the value of compassion and understanding will be ever-important as we traverse this learning curve together.
LOOKING AHEAD
With the abundance of new research on COVID-19, we still have much to learn about life during and after the virus. Optimistically, however, as we continue to dissect the research, our scientific community will highlight better ways to prevent, screen, and treat COVID-related complications moving forward.
**Receiving accurate information is the first step to a brighter future.
If you have recovered from COVID-19, and feel that you have experienced psychological or cognitive changes as a result of the virus, consulting for a neuropsychological evaluation may be appropriate to assess your current level of functioning – which can support a more personalized understanding of your recovery. To ask questions or discuss your concerns further, please contact us at: (805) 966-6197.
—And as always, remember our informal motto written below:
References
1. Couzin-Frankel, J. (2020). From ‘brain fog’ to heart damage, COVID-19’s lingering problems alarm scientists.
2. Kennedy, M., Helfand, B. K., Gou, R. Y., Gartaganis, S. L., Webb, M., Moccia, J. M., ... & Inouye, S. K. (2020). Delirium in Older Patients With COVID-19 Presenting to the Emergency Department. JAMA network open, 3(11).
3. Liotta, E. M., Batra, A., Clark, J. R., Shlobin, N. A., Hoffman, S. C., Orban, Z. S., & Koralnik, I. J. (2020). Frequent neurologic manifestations and encephalopathy‐associated morbidity in Covid‐19 patients. Annals of clinical and translational neurology, 7(11), 2221-2230.
4. Oliu-Barton, M., Pradelski, B. S., Aghion, P., Artus, P., Kickbusch, I., Lazarus, J. V., ... & Vanderslott, S. (2021). SARS-CoV-2 elimination, not mitigation, creates best outcomes for health, the economy, and civil liberties. The Lancet.
5. Taquet, M., Geddes, J. R., Husain, M., Luciano, S., & Harrison, P. J. (2021). 6-month neurological and psychological outcomes in 236,379 survivors of COVID-10: A retrospective cohort study using electronic health records. The Lancet.
6. Yamamoto, N., et al. “SARS-CoV-2 Infections and COVID-19 Mortalities Strongly Correlate with ACE1 I/D Genotype.” Elsevier, Gene 758. doi: https://doi.org/10.1016/j.gene.2020.144944
7. Zhou, H., Lu, S., Chen, J., Wei, N., Wang, D., Lyu, H., ... & Hu, S. (2020). The landscape of cognitive function in recovered COVID-19 patients. Journal of Psychiatric Research, 129, 98-102.